Common ICU Admission Diagnosis: An In-Depth Analysis

Common ICU Admission Diagnosis
Critical Care Statistics
Common ICU Admission Diagnosis: Over 16,000 highly trained professionals from more than one hundred countries are members of the Society of Critical Treatment Medicine (SCCM). These specialists offer treatment in specialized units. And strive to achieve the best possible results for all patients who are critically sick or wounded.
Multidisciplinary care teams are directed by intensivists, who are physicians who have received training. And credentials in critical care medicine (CCM), are vital to the delivery of critical care. According to the Society for Critical Care Medicine (SCCM).
These teams also enhance the working conditions of healthcare personnel. And raise the financial performance of hospitals. There are a lot of current problems in critical care in the United States. This guide includes statistics on many of those problems. The purpose of this document is to serve as a reference for activities such as advocacy, public relations, and general education.
Common ICU Admission Diagnosis: Expensiveness of Intensive Care
This represents a 92% rise in annual CCM expenses, which went from $56.6 billion to $108 billion between the years 2000 and 2010. While the charges in 2010 reckoned for 13.2 of sanitarium costs,4.1 of public health expenditures, and 0.72 of gross domestic product, the costs are significant. As of 2010, it was anticipated that the cost per day for intensive care unit (ICU) services would be $4300, representing a 61% rise over the cost per day in the year 2000, which was $2669.
Potential Reduced Expenditures
When it comes to critical care management of severe sepsis, and acute respiratory failure. And general critical care interventions. It is possible to achieve cost savings of up to one billion dollars for each quality-adjusted life-year gained. Several benefits are attributed to the utilization of intensivist personnel that are available around the clock.

These benefits include a reduction in expenses, mortality, complications, length of stay (LOS) in the hospital, enhanced physician satisfaction, and a reduction in burnout. Nevertheless, the vast majority of research studies highlight the advantages of intensivist staffing. That is available around the clock was carried out predominantly at university or tertiary hospitals. They must have a high patient volume and a high level of severity.

The utilization of an intensivist-directed multidisciplinary team in the delivery of treatment has the potential to result in yearly cost savings of up to thirteen million dollars for the hospital. The example of a community hospital that achieved a return on investment of 105% by implementing mandatory intensivist consultation and admission standards is illustrative of the impact that this type of care has.

As a result, the intensive care unit length of stay (LOS), ventilator-associated events, and central venous access device infection rates were all reduced.
The use of telemedicine or tele-intensive care unit services, in which sophisticated electronic systems connect intensive care unit patient data to intensivists located in remote places, may be beneficial to hospitals that do not have on-site intensivist care.
Common ICU Admission Diagnosis: Potential Reduced Expenditures
Additionally, the intensivists collaborate with the nurses at the bedside to provide services such as real-time monitoring, diagnostics, and intervention. Additionally, intensivists in telemedicine engage with patients as well as members of the patient’s families. Tele-intensive care unit (ICU) care has been shown to reduce the length of stay (LOS) in the intensive care unit (ICU) and the mortality rate in the ICU in some circumstances.

This might potentially result in reduced hospital expenses and improved utilization of available resources. Tele-intensive care unit (ICU) programs were related to decreases in ICU and hospital mortality as well as ICU length of stay (LOS), but not in hospital length of stay (LOS), and they were expensive to establish, according to the findings of a systematic review and meta-analysis of 19 ICU telemedicine studies.

Research that was conducted not too long ago by the Emory Critical Care Center revealed that the adoption of an advanced practice provider (APP) residency program and tele-intensive care unit (tele-ICU) that was staffed by critical care nurses and consultant intensivists resulted in a cost reduction expenditure of $4.6 million.
Those Patients in Critical Care
More than five million patients are admitted to intensive care units (ICUs) in the United States each year for specific reasons, including intensive or invasive monitoring, support of the airway, breathing, or circulation, stabilization of acute or life-threatening medical problems, comprehensive management of injury and/or illness, and the maximization of comfort for patients who are going to die.

Intensive care unit (ICU) patients are a diverse group, but they all have the same requirement for regular evaluation and a larger requirement for technology assistance than patients who are admitted to beds that are not in the ICU.
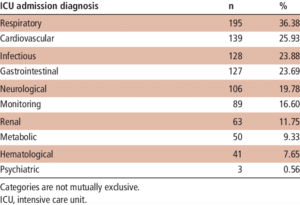
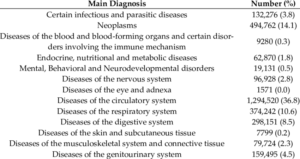
Adult: Conditions related to the heart, lungs, and nervous system are frequently seen in adult intensive care unit patients. For adults, the five most common reasons for admission to the intensive care unit are respiratory insufficiency or failure with ventilator support, acute myocardial infarction, intracranial hemorrhage or cerebral infarction, percutaneous cardiovascular operations, and septicemia or severe sepsis without the use of mechanical ventilation.
Common ICU Admission Diagnosis: Those Patients in Critical Care
Additional conditions and procedures that involve high utilization of the intensive care unit. Including poisoning and the toxic effects of drugs. Pulmonary edema, respiratory failure, heart failure and shock, cardiac arrhythmia, and conduction disorders. Renal failure with major complications or comorbidities, gastrointestinal hemorrhage with complications or comorbidities. And diabetes with complications or comorbidities.

Mechanical ventilation, which is required by twenty percent to forty percent of intensive care unit admissions in the United States, is the most prevalent kind of technology assistance.
About pediatrics, patients who are admitted to the pediatric intensive care unit (PICU) may be suffering from acute illnesses or acute exacerbations in the setting of complicated chronic disorders. The majority of patient diagnoses are related to respiratory conditions.

A child’s age spans from less than one year to 1.9 years when they are admitted to the pediatric intensive care unit (PICU). When it comes to the reasons for admission to the pediatric intensive care unit (PICU), the most prevalent ones are respiratory disease, heart disease, and neurologic diseases.

As many as 38 percent of pediatric intensive care unit admissions are made up of children who have developmental delays. More than 35–40% of patients who are admitted to the PICU have a length of stay (LOS) that is higher than seven days, and more than 40 40 of these patients require mechanical breathing.
A frequency of more than 8% globally and a fatality rate of more than 24% are associated with severe sepsis and septic shock, both of which are prevalent in pediatric intensive care units (PICUs).
Common ICU Admission Diagnosis: Those Patients in Critical Care
Patients born prematurely or at term are admitted to the neonatal intensive care unit (NICU). They are those who have been diagnosed with significant medical or surgical issues. More than half of the infants were admitted to the neonatal intensive care unit (NICU). They were born at term and had normal birth weights. This is even though the majority of very-low-birth-weight (< 1500 g) neonates are cared for in NICUs.

When a neonatal intensive care unit (NICU) is present at a facility, the outcomes for high-risk babies, particularly preterm infants, are improved. From 4% to 46% in industrialized nations, the mortality rate in neonatal intensive care units (NICUs) ranges from 0.2% to 64.4% in impoverished countries.
According to the definition provided by the American Academy of Pediatrics (AAP). A neonatal intensive care unit (NICU) is a facility that is capable of providing newborn care that includes sustained life support. A full spectrum of respiratory support, access to pediatric medical and surgical specialties, both pediatric anesthesiologists and pediatric ophthalmologists.

The Neonatal Intensive Care Unit (NICU) is defined by the American Academy of Pediatrics (AAP). As are four different levels of care, with the capabilities rising as the level increases. Level I is a well-baby nursery, and level 2 is a special-care nursery. Levels III and IV are full intensive care unit care.
Common ICU Admission Diagnosis: The Facilities of the Intensive Care Unit
The American Hospital Association (AHA) Hospital Statistics System and the United States Centers for Medicare. And Medicaid Services Healthcare Cost Report Information System (HCRIS) are the two national hospital databases. This provides accessibility to information on intensive care unit (ICU) facilities in the United States.

In addition to providing information on the number of intensive care unit beds and units for burn units. And observation, step-down, or progressive beds. The American Heart Association (AHA) also provides statistics on the number of adults (medical-surgical, cardiac, and other). And child (pediatric and neonatal) units. No data on bed use is provided by the AHA.

Bed and utilization statistics are available for adult (intensive care, coronary care, surgical/trauma, burn, psychiatric/detoxification). And child (pediatric and neonatal) beds through the Health Care Information and Resource Information System (HCRIS), but not on units. Medicare and Medicaid use in the United States government are included in the HCRIS statistics. When it comes to observation, step-down, or progressive beds, HCRIS does not have any statistics.
There were 4862 acute care registered hospitals in the United States, according to the American Hospital Association’s (AHA) annual survey from 2015. Of these hospitals, 2814 had at least 10 acute care beds and at least one intensive care unit bed.

There were a total of 540,668 staffed beds in these hospitals. And there were 94,837 intensive care unit beds (14.3% of total beds) in 5229 intensive care units.
In all, there were a total of 46,490 medical-surgical beds spread across 2644 units. 14,731 cardiac beds spread across 976 units. And 6588 other beds spread across 379 units, 4698 pediatric beds spread across 307 units. And 22,330 neonatal beds spread across 920 units.
Common ICU Admission Diagnosis: Intensive Care Unit
In the medical-surgical, cardiac, and other units, the median number of beds was 12. While the number of beds in the newborn and pediatric units was 18 and 10 respectively. Half of the hospitals had one unit, twenty-four percent had two units, and twenty-four percent had three or more units.

According to data from HCRIS, 2977 acute care hospitals had intensive care unit beds in 2010. Among them, there were 103,900 intensive care unit beds. Which accounted for 16.2% of the total number of beds in the intensive care unit.
In the United States, the number of beds in critical care facilities climbed by 17.8 percent between the years 2000 and 2010, going from 88,235 to 103,900. However, the majority of the expansion is in the supply of critical care beds. This is taking place in a limited number of locations in the United States.

These places often have large populations and a lower number of intensive care units (ICUs) per 100,000 people. A greater occupancy rate in the ICUs at the beginning of the study. And increasing market rivalry. In addition, between the years 2000 and 2010. The beds for neonates saw the highest percentage growth, which was 29%, followed by beds for adults, which was 26%.
Facilities Available In The Intensive Care Unit
The beds for children experienced the least amount of change, which was 2.7%. In 2010, there were 103,900 intensive care unit beds, of which 83,417 (80.3%) were reserved for adults, 1917 (1.8%) were reserved for children, and 18,567 (17.9%) were reserved for neonates.

Overall, there were 33.6 beds for every 100,000 people. 35.5 beds for every 100,000 adult beds (for those older than 18 years). Also, 2.7 beds for every 100,000 pediatric beds (for those between the ages of 1 and 17 years). And 470 beds for every 100,000 neonatal beds (for those less than one year).
There were 150.9 million hospital days in 2010, with 25 million spent in the intensive care unit (ICU). This is 16.5% of the total number of days spent in the hospital. The number of intensive care unit days that Medicare covered was 7.9 million (31.4%), while Medicaid covered 4.3 million (17.2%).

The occupancy rates were determined using the HCRIS data (days/possible days) to compute the occupancy rates. Equally important, In 2010, the occupancy rates of hospitals and intensive care units were 64.6% and 68.